Miller Fisher Syndrome (MFS) is considered a rare nerve disease that can be acquired following occurrences of viral infections. The disease affects the central nervous system which attacks the body’s own auto-immune system. The autoimmune disorder happens when healthy body tissues are mistakenly attacked by the immune system such as in the case of Miller Fisher Syndrome. The myelin sheath which acts as a nerve insulator in the central nervous system is attacked and destroyed by the immune system. This result is known as demyelination. In this condition the signals are disrupted between the brain and other parts of the body
Miller Fisher Syndrome was discovered by Dr. Charles Miller Fisher in 1956, a Canadian stroke neurologist. The MFS disease is the variant form of Gullain Barre Syndrome (GBS). Gullain Barre Syndrome commonly occurs than the MFS. MFS is a rare disease since it only affects 1 person per 2,000. There are other names for the Miller Syndrome, Miller Fisher Variant of GBS, Fisher’s syndrome and acute idioplastic ophthalmologic neuropathy.
Symptoms of Miller Fisher Syndrome
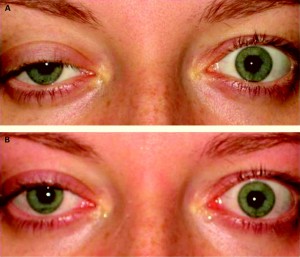
MFS is characterized by the inability of the muscles to coordinate properly (ataxia), absence of the tendon reflexes (areflexia), and paralysis of the eye muscles (ophtalmoplegia) which causes impaired vision, and sensitivity to light. Other symptoms that can be observed are total muscle weakness in the body and failure of the respiratory system.
Causes of Miller Fisher Syndrome
There is no known fact about the cause of MFS but studies show two thirds of those who had MFS, suffered viral infections prior to the disease. Some of them experienced diarrhea, colds and sore throat before the onset of the Miller Fisher Syndrome. It was also observed that many patients who suffered MFS suffered an infection of Campylobacter jejuni before they acquired the disease. Campylobacter jejuni is a curved, non-spore forming, Gram-negative bacterium which is commonly found in animal feces.
Diagnosis and Treatment of Miller Fisher Syndrome
Cerebrospinal fluid testing (CSF), electromyography (EMG) and nerve conduction study (NCS) are usually conducted to diagnose the Miller Fisher syndrome. The purpose of the tests is to assess and confirm the symptoms. The clinical findings noted in these tests are the basis for treatment options.
One of the most important aspects of treatments for MFS is full attention and dedicated support to the patient. Vital functions of the limbs; any sign of failure or problems with the respiratory system which usually occurs after the paralysis of the diaphragm, and early intubation should be carefully monitored. The treatment of Miller Fisher Syndrome includes medication of immunoglobulins given intravenously. Other treatments such as Plasmapheresis and physical therapy are applied to treat motor symptoms. In the treatment process, patients undergo rehabilitation. Recovery takes time and patients should be monitored for their physical movements for them to regain lost functions. After tracheotomy, occupational and speech and language therapy are usually applied.
Patients with Miller Fisher Syndrome have good chances of fully recovering their motor skills. Usually within 2 to 4 weeks of the onset of symptoms, patients start to recover. And within 6 months they will be able to live normally. A relapse may happen but this is seldom.
Have Miller Fisher overlapped with Becker staff brain stem ay now for three years. My muscles feel like they are stretched to areturn to nor limit before they will snap. My gait is severely affected due to my muscle tightness. I get extremely tired very quick. Everyday activities are affected is cannot climb a ladder, drive a car, write my name etc. Will I ever return to normal? My Doc gave me dates of 6 months, then 1 year, then 2 years, and now he says do not know. That I had a very servere case of MFS