Ulcerative Colitis is the swelling of the large intestine and is characterized by ulcers on the lining of the colon, which eventually leads to bleeding and production of pus. The inflammation also results to frequent emptying of the colon, causing diarrhea. Patients with Ulcerative Colitis alternate between periods of stomachaches and diarrhea accompanied by mucus, blood and pus; and periods showing few or no symptoms at all.
Ulcerative Colitis affects all age groups, though more cases are found in the 15 to 30 year-old bracket; while less frequent in those aged 50 to 70 years old. Women are 30 percent more susceptible to it than men. The risk of having this disease is higher when you have a relative that has this. Cases of this disease are rare in the UK, with only one per 10,000 individuals diagnosed annually. Asians also rarely acquire this disease.
Ulcerative Colitis Symptoms
The manifestations of this disease differ from one case to another. As previously mentioned, there are alternating periods showing few or no symptoms, and periods of stomach pain, diarrhea with blood, mucus and pus. Symptoms also differ depending on the degree of the disease. For cases where the disease is only affecting the rectum, the symptoms are relatively mild. In about one-third of cases, the disease has spread to the lower part of the large intestine. While others still, have Ulcerative Colitis on the whole large intestine. About fifty percent of the patients show only mild symptoms. While other cases manifests recurring fever, diarrhea with blood, nausea and relentless stomach pain.
Other symptoms are the following:
• anemia
• fatigue
• growth failure (in children)
• joint pain
• loss of appetite
• loss of body fluids and nutrients
• rectal bleeding
• skin lesions
• weight loss
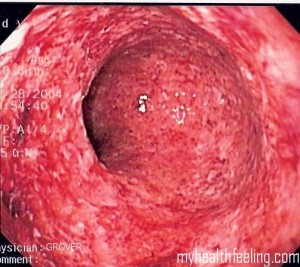
Ulcerative Colitis Pictures
Ulcerative Colitis Cause
The root cause of Ulcerative Colitis is not yet known. Various theories pointing to immunological, infectious and hereditary factors have been formulated. It should be noted that certain foods and emotional distress do not cause this disease, but may set off the symptoms.
Diagnosis of Ulcerative Colitis
To correctly diagnose Ulcerative Colitis, physicians conduct several tests. Below are the steps taken to diagnose this disease.
1. Medical history of the patient is taken and physical examination is primarily conducted.
2. Blood tests – These are done to check if there is bleeding and inflammation within the body. A high count of white blood cells may signify the latter, and a low hemoglobin count may mean the former.
3. Stool exams – The presence of white blood cells in the stool may indicate a swelling in the body. The presence of red blood cells means there is bleeding in the rectum or colon. The examination also allows for the elimination of other causes such as parasites and bacteria.
4. Sigmoidoscopy or Colonoscopy – These procedures make diagnosis of Ulcerative Colitis more definite. These tests involve the insertion of the endoscope to the anus, thus enabling the doctor to check the rectum and the colon. Should there be any swelling, ulcers and bleeding on the walls of the colon, these should be obvious on the monitor. A sample of the tissue from the colon wall could also be taken for biopsy. This will further confirm the presence of the disease.
5. Barium Enema X-ray – This may be done to know the degree of disease inside the colon and rectum. CT scans may also be conducted for the same purpose.
Ulcerative Colitis Treatment
Treatment varies from case to case, depending on the extent of the disease. Treatment regimen, therefore, is specific to each patient.
• Medication Therapy
If the disease is active, medication is given to resolve the symptoms. Even if the patient is in remission, taking in drugs is continued to improve the patient’s quality of life and maintain remission. Several drugs are prescribed for this.
o Aminosalicylates – These medicines help quell the inflammation. Depending on where the swelling is, they may be taken through the oral route, as a suppository or thru an enema. This group of drugs is the first ones given for mild to moderate cases. They are also administered in instances of relapse.
o Corticosteroids – These are anti-inflammatory drugs too, and are usually given to patients who do not respond to Aminosalicylates. For mild to moderate cases, suppositories and enemas are recommended. But for severe cases, tablets are ingested instead. These are very effective for short-term use but are not to be used for long periods of time as they cause many side effects.
o Immunomodulators – These are administered to patients who are not successful with either of the previously-mentioned drugs. These are taken orally. Relief, though, is not immediate and may take 6 months for the symptoms to be fully resolved. Constant monitoring for complications in patients is necessary.
Medications for infection, pain and diarrhea are also administered. There are cases of remission that lasts for months to years. But most cases see relapse after a while.
If drug therapy is not successful, hospitalization and surgery are other options. Surgery removes part or the whole large intestine, thus, curing Ulcerative Colitis.